The pros and cons of a hysterectomy are for individuals considering life-changing decisions to their anatomy and physiology.
This article is also for those who must have heard of this significant medical term and wish to know its meaning or to be informed for research purposes.
This article will help you understand life after surgery, potential complications during and after the procedure, and the pros and cons of a hysterectomy.
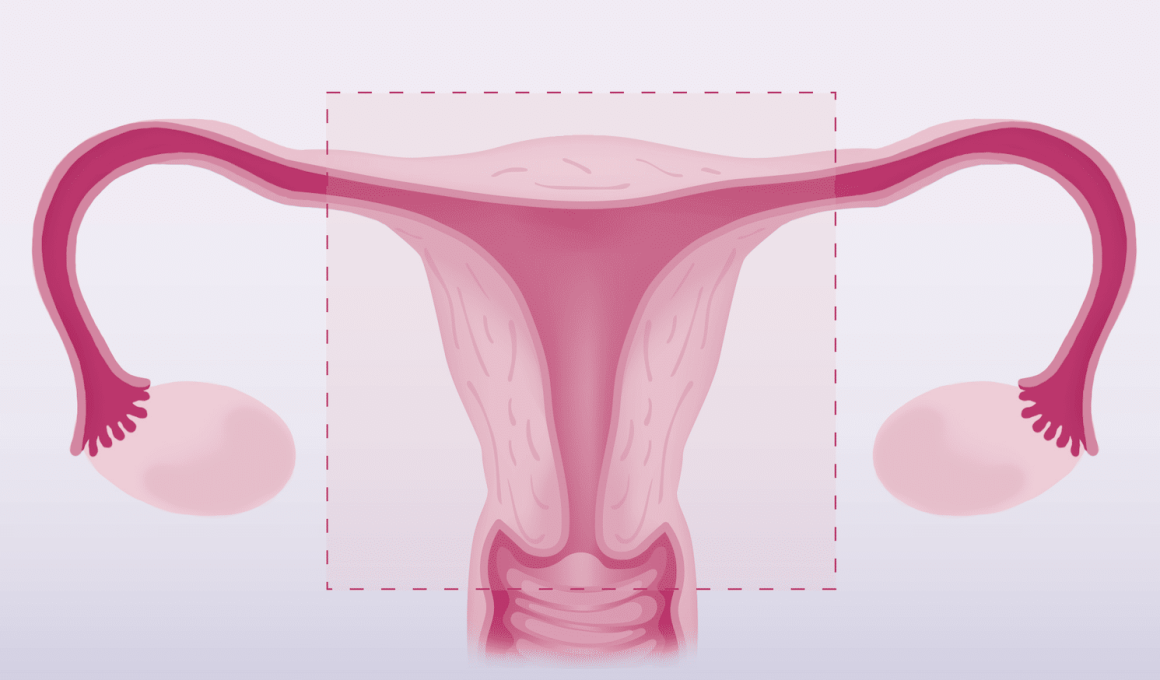
What is a Hysterectomy?
A hysterectomy is a major surgical procedure that involves the removal of the uterus or womb in women.
It is usually done to treat certain medical conditions, such as uterine fibroids, endometriosis, prolapse of the uterus, or cancer.
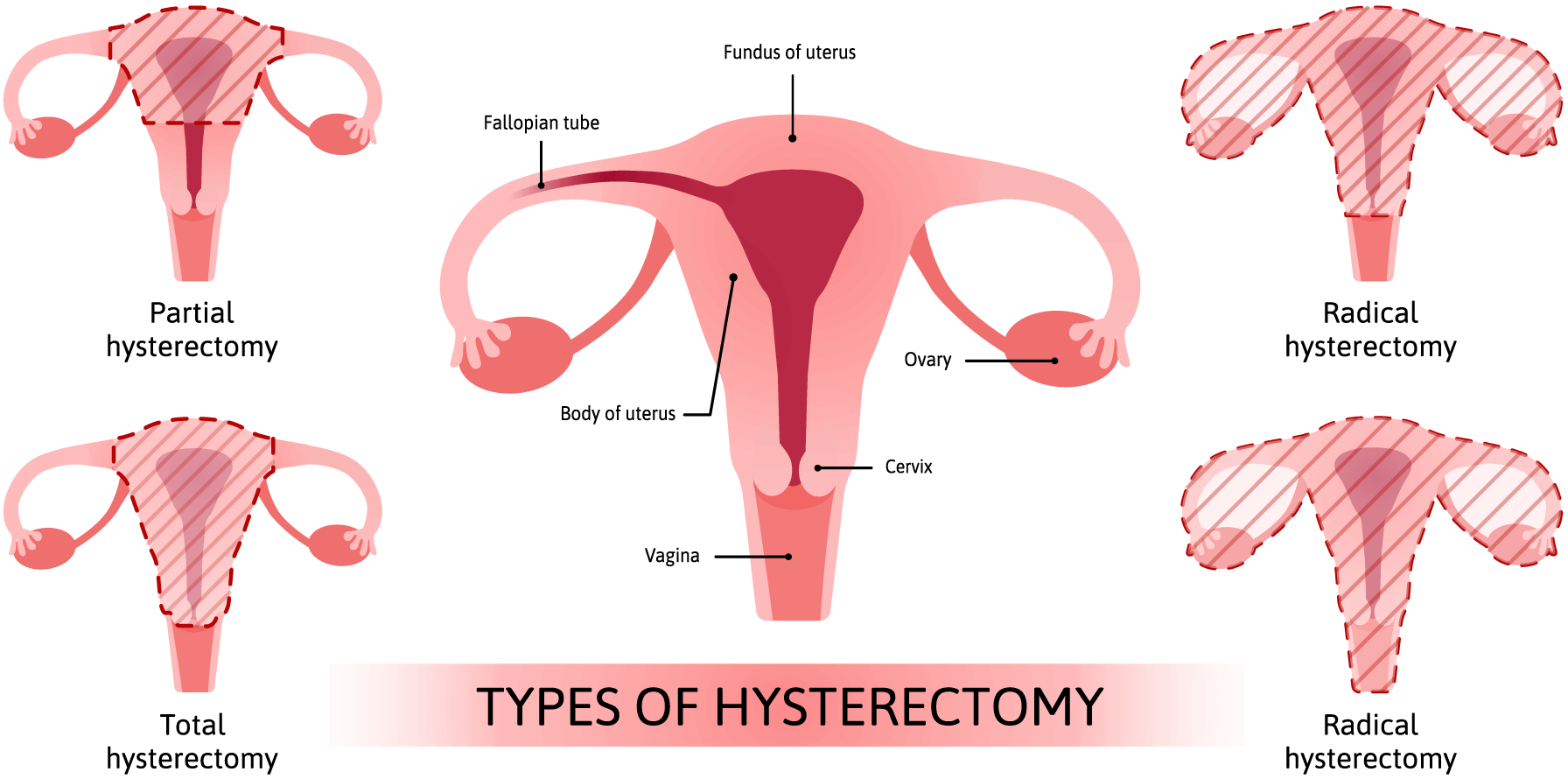
Hysterectomies can be partial (removal of only part of the uterus) or total (removal of the entire uterus).
Depending on the type of procedure, other reproductive organs, such as the ovaries and fallopian tubes, may be removed simultaneously.
A hysterectomy may be done through an open abdominal incision (abdominal hysterectomy) or laparoscopically (using a thin, lighted tube inserted through small incisions in the abdomen).
In some cases, performing a hysterectomy through the vagina is possible.
After a hysterectomy, most women experience some degree of physical recovery. The amount of time it takes to heal depends on the type of procedure that was performed.
Typically, patients can expect to return home on the same day as their surgery or within a few days.
Many factors influence recovery time and overall healing, such as age, general health, type of anesthesia used, and procedure.
Complications from a hysterectomy may include damage to organs ranging from mild to severe, bleeding, or damage to nearby organs.
Before deciding, it is essential to talk to your doctor about the potential pros and cons of a hysterectomy.
What Are the Types of Hysterectomies?
Various forms of hysterectomy can be performed depending on the patient’s needs.
The most common forms of hysterectomy are:
1. Abdominal Hysterectomy
Abdominal hysterectomy is a surgical procedure involving removing a woman’s uterus through an incision in the abdomen.
This type of hysterectomy may be recommended for various medical conditions, such as fibroids, endometriosis, or ovarian cancer.
While it is a major surgery requiring general anesthesia and hospitalization, it can relieve symptoms and improve overall health outcomes for some women.
During the surgery, an incision is made in the lower abdomen, and the uterus, and sometimes the cervix, are removed.
The surgeon may also remove the ovaries and fallopian tubes if there is a medical reason. After removing the uterus, the incision is closed with sutures or staples.
Recovery from an abdominal hysterectomy can take several weeks. Patients may experience pain, discomfort, and fatigue during this time.
They must rest and avoid heavy lifting or strenuous activity for several weeks after the surgery. Pain medication may be prescribed to manage discomfort.
2. Total Hysterectomy
A total hysterectomy is a medical procedure involving removing a woman’s uterus and cervix.
This surgery is typically recommended for women with certain medical conditions, such as uterine fibroids, endometriosis, or ovarian cancer.
While it can be an effective treatment option for these conditions, a complete hysterectomy is a major surgical procedure that requires careful consideration and preparation.
3. Partial/Subtotal Hysterectomy
A partial hysterectomy is a surgical procedure involving removing the uterus while leaving the cervix intact.
This type of surgery is typically recommended for women with fibroids, endometriosis, or abnormal uterine bleeding.
Unlike a total or complete hysterectomy, where the uterus and cervix are removed, a partial hysterectomy preserves the natural hormonal balance in women and does not affect sexual desires.
During a partial hysterectomy, the uterus is removed through incisions in the abdomen or vagina.
Depending on the case, the surgeon may remove the fallopian tubes and ovaries.
Recovery time for a partial hysterectomy is usually shorter than for a total hysterectomy, with most women returning to normal activities within a few weeks.
4. Radical Hysterectomy
A radical hysterectomy is a surgical procedure that removes the uterus, cervix, and some surrounding tissues.
It is commonly used as a treatment option for early-stage cervical cancer and other gynecologic cancers.
This procedure can be done through an open incision or minimally invasive hysterectomy such as laparoscopy or robotic surgery.
Radical hysterectomy can significantly affect a woman’s reproductive and sexual health and overall quality of life.
During a radical hysterectomy, the surgeon will remove the uterus, cervix, the upper part of the vagina, and some surrounding tissues.
In some cases, the ovaries and fallopian tubes may also be removed.
This procedure is usually performed under general anesthesia and can take several hours to complete.
5. Supracervical Hysterectomy
Supracervical hysterectomy is a surgical procedure involving removing the uterus while leaving the cervix intact.
This type of hysterectomy is becoming increasingly popular as it offers several benefits, including a quicker recovery time and a lower risk of complications than traditional hysterectomy methods.
However, it is crucial to understand the risks and benefits of supracervical hysterectomy before deciding if this option is right for you.
One of the main advantages of a supracervical hysterectomy is that it can be performed through smaller incisions, which reduces scarring and post-operative pain.
This also means patients can typically return to normal activities sooner than traditional hysterectomy methods.
6. Laparoscopic Hysterectomy
Laparoscopic hysterectomy is a minimally invasive surgical technique used to remove the uterus.
In this procedure, a laparoscope – a thin, lighted tube with a camera on its end – is inserted through small incisions in the abdomen.
The surgeon then uses specialized tools to carefully detach the uterus from surrounding tissues and remove it through one of the small incisions.
Compared to traditional open surgery, laparoscopic procedures offer several benefits, including less pain and scarring, shorter hospital stays, and faster recovery times.
This procedure is typically recommended for women requiring a hysterectomy due to fibroids, endometriosis, or cancer.
It may also be used in cases where a traditional open surgery would pose too great a risk due to factors such as obesity or prior abdominal surgery.
7. Robotic Hysterectomy
A robotic hysterectomy is a minimally invasive surgery in which an automated system assists the surgeon during the operation.
The robotic system consists of a console with a control panel.
The surgeon sits and operates the instruments and robotic arms inserted into the patient’s abdomen through small incisions.
The robotic arms are equipped with tiny instruments and a high-definition camera, providing the surgeon with a 3D view of the surgical site.
The surgeon uses hand and foot controls to manipulate the instruments, which have more excellent skill and range of motion than human hands.
The benefits of robotic surgery are numerous. Because it is minimally invasive, there is less pain and scarring than in traditional open surgery.
8. Vaginal Hysterectomy
A vaginal hysterectomy is a surgical procedure involving removing the uterus through the vagina.
It is one of the most common types of hysterectomies and is often preferred over other methods due to its minimally invasive nature and shorter recovery time.
During a vaginal hysterectomy, the uterus is detached from its surrounding tissues and blood vessels.
The surgeon then removes the uterus through an incision made in the vagina.
Unlike other types of hysterectomies that require larger incisions, this procedure only requires a small one in the vaginal wall.
Recovery from a hysterectomy can vary depending on the type of procedure that was performed.
Generally, full recovery is expected within 4-6 weeks for laparoscopic surgery and robotic hysterectomy and up to 8 weeks for more invasive hysterectomy procedures such as the radical technique.
During recovery, it is paramount to follow your doctor’s instructions for rest and activity and any additional treatments that may be recommended.
What to Consider Before Having a Hysterectomy?
When considering a hysterectomy, it is crucial to understand why it is recommended.
A hysterectomy may be recommended for various reasons, including removing cancerous or pre-cancerous, heavy bleeding, fibroids, endometriosis, chronic pelvic pain, and prolapsed uterus.
Discuss with your doctor the potential pros and cons of a hysterectomy and any alternative treatments that may be available.
Another vital factor to consider when deciding whether or not to have a hysterectomy is your age.
Discuss fertility preservation options with your doctor if you are in your childbearing years and desire to become pregnant.
It is also essential to consider the long-term implications of a hysterectomy.
For example, a hysterectomy may cause menopause to occur earlier than it would have naturally, resulting in an increased risk of osteoporosis and other major complications.
Finally, discuss your financial situation with your doctor and insurance provider before having a hysterectomy.
Insurance may cover a hysterectomy in some cases but know that any out-of-pocket costs may incur.
A hysterectomy is a major surgical procedure that can significantly affect women’s health.
Before deciding to have a hysterectomy, consider all your options and be aware of the potential risks and benefits of the procedure.
Additionally, discuss your age, fertility preservation options, long-term implications, and financial considerations with your doctor before deciding.
Pros of a Hysterectomy
Although significant risks are associated with surgery, potential benefits may make the procedure desirable.
Although there are more, some common pros and cons of a hysterectomy are below.
1. Relief of Symptoms
One of the most common reasons for a hysterectomy is to relieve painful and disruptive symptoms caused by medical conditions such as endometriosis or uterine fibroids.
Many women with a hysterectomy report significant pain relief and improved quality of life after the procedure.
2. Reduced Risk of Cancer
A hysterectomy can also reduce the risk of developing certain cancers, such as ovarian and endometrial cancer.
Women with a family history of these types of cancer may be more likely to benefit from this procedure.
Also, a hysterectomy can help detect pre-existing conditions that could increase cancer risk.
3. Easier Menopause
For some women, a hysterectomy can make menopause easier to manage.
Removing the uterus eliminates the production of hormones associated with menstruation, which can help reduce symptoms such as hot flashes and vaginal dryness that are common during menopause.
4. Improved Quality of Life
A hysterectomy can relieve uncomfortable and disruptive symptoms, leading to an improved quality of life.
Women with a hysterectomy often feel more confident and in control of their bodies.
5. No More Worries About Pregnancy
One of the main advantages of a hysterectomy is that it eliminates the risk of pregnancy.
This can be especially beneficial for women who do not wish to become pregnant or are done having children.
Also, if a woman has had multiple pregnancies, a hysterectomy may help reduce her risk of developing pelvic prolapse.
6. Improved Sexual Function
After a hysterectomy, some women also report an improved sex life. This can be due to the relief of symptoms such as mild to severe pain during intercourse or vaginal dryness.
Plus, after the procedure, some women feel happier and in control of their bodies, which may lead to improved sexual function.
7. Less Risk of Infection
A hysterectomy can also reduce the risk of certain infections, as it eliminates the uterus and cervix, which are common sites for disease.
Women who have had a hysterectomy may be less likely to experience chronic pelvic pain due to decreased bacteria in the reproductive tract.
8. Improved Mental Health
Hysterectomies can positively impact mental health, as they may help reduce anxiety and depression associated with disruptive symptoms or the fear of developing certain types of cancer.
Women who feel in control of their bodies after the procedure have improved well-being.
This shows that a hysterectomy can relieve worries such as becoming pregnant or dealing with menstrual cycles.
9. Reduced Risk of Uterine Issues
A hysterectomy can also reduce the risk of developing specific uterine issues, such as cysts and fibroids.
It is important to note that these conditions can still develop after a hysterectomy but are less likely to occur.
A hysterectomy eliminates the risk of uterine prolapse, which can cause significant discomfort.
10. Fewer Complications
Hysterectomies are generally safe procedures that have a low risk of complications.
If the uterus is removed, it eliminates the risk of uterine cancer and other conditions associated with the uterus.
Furthermore, a hysterectomy can reduce the risk of preterm labor and certain vaginal infections.
11. Cost-Effectiveness
Hysterectomies are generally cost-effective procedures, as they eliminate the need for regular medical check-ups and surgeries that may be necessary to treat uterine issues.
Cons of a Hysterectomy
1. Early Menopause
If your ovaries are removed during the hysterectomy, you may experience early menopause. This can cause symptoms such as hot flashes, night sweats, vaginal dryness, and mood swings.
2. Reduced Sexual Pleasure
Hysterectomy can affect sexual desires in some women. Removing the uterus and ovaries can reduce libido and cause vaginal dryness, making sex painful or uncomfortable.
3. Increased Risk of Urinary Incontinence
Hysterectomy can damage the pelvic floor muscles and nerves, leading to urinary incontinence (involuntary urine leakage).
This can be a particularly distressing complication for women with other health issues.
4. Risk of Complications During Surgery
Like any surgical procedure, a hysterectomy carries some risks. These can include bleeding, infection, damage to surrounding organs, and anesthesia complications.
5. Emotional Impact
Hysterectomy can have a significant emotional impact on women, particularly those who may feel they are losing a part of their identity as a woman or who have concerns about fertility.
6. Long-term Health Effects
Some evidence suggests that women undergoing a hysterectomy may be at increased risk of developing certain health conditions later in life, such as cardiovascular disease and osteoporosis.
7. Hormone Replacement Therapy
If your ovaries are removed during the hysterectomy, you may need hormone replacement therapy (HRT) to manage menopausal symptoms and reduce the risk of other health problems.
However, HRT carries its risks, including an increased risk of breast cancer, stroke, and blood clots.
8. Surgical Menopause
Women who undergo a hysterectomy with both ovaries removed will experience surgical menopause immediately after the surgery.
This can cause severe hot flashes, night sweats, and other menopausal symptoms that may be difficult to manage.
9. Impact on Future Fertility
One of the biggest cons of a hysterectomy is that it can impact a woman’s ability to have children in the future.
If only the uterus is removed, some women may still be able to conceive with the help of assisted reproductive technologies like IVF.
However, if both ovaries are removed, this may not be possible without donor eggs.
10. Impact on Mental Health
Having a hysterectomy can also have an impact on a woman’s mental health. It may lead to sadness, grief, or loss, especially for those who had hoped to have children.
This emotional burden can be challenging for women dealing with other health issues.
11. Recovery Time
Recovering from a hysterectomy can take time, and women may need to take several weeks off work or other activities to allow their bodies to heal.
The recovery process can be painful and uncomfortable, with some women experiencing cramping, bleeding, and discomfort for several weeks after the surgery.
12. Cost
Hysterectomy is a major surgical procedure that can be expensive, mainly if it requires an extended hospital stay or other complications.
Women should check with their insurance providers to determine what costs are covered and explore alternative, more cost-effective treatment options.
Conclusion
Considering all the potential pros and cons of a hysterectomy is essential.
Women should discuss their concerns with their healthcare provider and explore possible alternative treatments.
Weigh the potential benefits of the surgery against the risks, particularly for women dealing with chronic pain or other medical conditions.
Ultimately, each woman’s decision about whether or not to have a hysterectomy should be based on her health needs and goals.